The netherlands country report a different route to success
Bạn đang xem bản rút gọn của tài liệu. Xem và tải ngay bản đầy đủ của tài liệu tại đây (427.15 KB, 9 trang )
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
The Netherlands Country Report
A different route to success
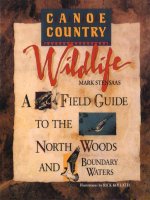
Mental Health Integration Index Results
Mental Health Integration Index:
Results for Netherlands
Netherlands
Best
Average
Worst
Environment
Governance
100
80
60
40
20
Overall:
Environment:
Opportunities:
Access:
Governance:
72.8/100 (7th of 30 countries)
90.0/100 (3rd)
77.8/100 (5th)
72.0/100 (7th)
53.3/100 (15th)
Other Key Data
0
20
40
60
80
100
Access
Opportunities
l Spending: Mental health budget as proportion of
government health budget (2009): 11%.
l Burden: Disability-adjusted life years (DALYs) resulting from
mental and behavioural disorders as proportion of all DALYs
(World Health Organisation estimate for 2012): 13.5%.
l Stigma: Proportion who would find it difficult to talk
to somebody having a serious mental health problem
(Eurobarometer 2010): 17%.
Highlights
The Netherlands ranks high in The Economist Intelligence
Unit’s Mental Health Integration Index, coming
seventh overall. 3rd in the Environment category, 5th in
Opportunities, and 7th in Access.
The evolution of the system has been unusual: the country
created an extensive parallel system of community care
without doing much do reduce hospital-based provision.
A series of mergers in the 1990s between hospitals and
community care groups created organisational integration
of provision.
SPONSORED BY
1
Government financial incentives—the most frequently used policy
lever—helped give primary-care providers a large role in mental
healthcare provision.
These developments collectively created the largest mental
health workforce in the Index, but the relatively high number of
individuals using these services has raised cost concerns.
A major reform of the Dutch healthcare system in 2006, combined
with a lack of overarching government policy, has improved
provision for those with moderate mental illness, but not those
with more severe cases.
The current environment also encourages extensive innovations,
which are worth examining.
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
The Netherlands ranks highly in the Mental Health Integration
Index, ranking in seventh place overall. It also does very well
in several specific areas covered by the index, including in the
“Environment” category (which measures the existence of
policies allowing those with a mental illness to lead a stable
home and family life), where it is placed third. It is ranked in
fifth place in the “Opportunities” category (which covers issues
surrounding employment) and seventh for “Access” (which
looks at the availability of medical care).
A different road to community care
Rene Keet, a psychiatrist and director of the Mental Health
Centre, GGZ North Holland, agrees that his country has
“well organised mental healthcare system that works so it is
accessible to everyone”. Frank van Hoof, senior scientist at
the Trimbos Instituut—a centre of expertise on mental health
and addiction—adds that in the Netherlands “there is less
negligence of the basic needs [of people living with mental
illness] than in some other countries. They are taken care of in
a good way.”
The process began in 1974 amid an intellectual environment
favourable to anti-psychiatry. A new government policy sought
to create a second tier of mental healthcare between primary
care and psychiatric hospitals, including social psychiatric
services, multi-disciplinary psychotherapy units, and even
family and marital guidance counsellors. In 1982 the Dutch
integrated the resultant patchwork system into 59 regional
centres for mental health outpatient care, at the same time
also devolving responsibility for such provision to the local
level. The ethos of these aggregate institutions was very much
on the psycho-social side of mental healthcare.
Nevertheless, both stress that Dutch healthcare and services
for this group have weaknesses as well as strengths. Despite
recent increases in the number of people having treatment,
currently an estimated three-quarters of those with some
mental health issue, and one-quarter of those with a serious
condition, receive no treatment.1 Moreover, the Netherlands
has a number of unusual attributes for a country that does
so well in the Index, including one of the highest number of
psychiatric hospital beds per head in Europe and a lack of any
overarching national government policy on mental health.
An unusual evolution helps to explain the current state of
provision.
Several European countries serve as cautionary tales for overrapid deinstitutionalistion, where reformers—or politicians
seeking savings—shut psychiatric hospitals before putting in
place effective, community-based provision. The Netherlands
is a mirror image of this: it created an extensive supply of
outpatient care while only slightly reducing institutional
provision.
Unfortunately, recalls Dr Keet, these major developments
in services “did not reach the psychiatric hospitals, which
went on doing the same things as before”, and until recently
retained their one-sided biomedical orientation. Bed numbers
remained roughly constant into the 1990s, even as they
declined in several other European countries. Moreover,
continuity of care between hospitals and regional centres
was at first practically non-existent, leaving any serious
cases discharged from hospital into the community with poor
provision. This problem worsened in the mid-1990s, when a
new mental health law raised the bar for both involuntary and
The overall figures are frequently cited, but those for serious conditions
come from Philippe Delespaul et al, “Consensus over de definitie van mensen
met een ernstige psychische aandoening (epa) en hun aantal in Nederland”,
Ttijdschrift voor Psychiatrie (2013).
1
2
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
voluntary admission to hospital. The situation engendered
substantial public criticism of mental healthcare.
Accordingly, the government encouraged greater integration
through voluntary arrangements between providers. It also
created special financing arrangements, covering all of mental
healthcare directly under the Exceptional Medical Expenses Act
(AWBZ), which, in other medical fields, normally paid only for
long term care. Although operating through regional offices,
this system followed clear national guidelines giving the
government a useful policy lever. The arrangement led to lower
average pay for mental healthcare providers than other health
professionals and, some also believe, increased stigmatisation
of those with mental illness.2 Nevertheless, it had the positive
effect of encouraging integrated thinking in the sector.
Beginning in the mid-1990s and accelerating towards the
end of the decade, this environment and the exigencies of
providing care led to a large number of mergers between
regional centres, hospitals, and other specialist mental health
organisations to create integrated care providers.
After further mergers throughout the last decade, 33 of
these largely private—both non-profit and commercial—
entities now provide roughly 85% of Dutch secondary mental
healthcare.3 As the Index shows, home care and assertive
community treatment are available in the Netherlands, but
these integrated groups provide a far wider range of offerings,
including: sheltered housing, non-psychiatric residential
facilities, assisted living services, as well as acute and longterm inpatient hospital care.
The role of psychiatric hospitals as an integral part of these
organisations, however, has limited the decline in psychiatric
bed numbers compared with the drop experienced in other
Maarten Van Schijndel et al, “The state of psychiatry in the Netherlands:
Strength by quality, influence by capabilities”, International Review of
Psychiatry, 2012.
2
GGZ Nederland, “Mental Healthcare in the Netherlands Key Figures 2012”,
2014 [ />Dutch%20specialist%20mental%20health%20care.pdf]; Frank van Hoof et al,
Outpatient care and community support for persons with severe mental health
problems: A comparison of national policies and systems in Denmark, England
and the Netherlands, 2011.
3
3
countries. After an 18% fall between 1997 and 2003—the
high point of merger-led consolidation—the figure has
remained stable at around 140 per 100,000, now the highest
in Europe after Belgium. Moreover, the majority of these
beds (60%) are long-stay ones, often in buildings that began
as traditional psychiatric hospitals far from population
centres.4 In that sense, says Mr van Hoof, “there has not been
deinstitutionalisation”. It is instead the much more rapid
expansion of non-residential facilities and services that has
given community-based mental healthcare in the Netherlands
a dominant weight, with the large majority of secondary
mental healthcare, including 89% of all care and 60% of that
for the most serious mental illnesses, being ambulatory,
outpatient provision.5
Moves towards greater integration with mainstream
medicine
For many years, Dutch mental healthcare stood apart from
the mainstream medicine and the anti-psychiatry movement
further isolated it. The last two decades, however, have seen
a shift towards greater integration in several ways, driven in
part by government policy—typically enacted through the
provision of strategic funding rather than direct intervention—
but also by greater co-operation between psychiatry and
other disciplines in creating evidence-based approaches to
treatment.
Among the most visible results has been the development of
a substantial level of treatment and diagnosis at the primarycare level, with general practitioners (GPs) having a gatekeeper
role for other types of provision. Around 80% of those seeking
help for a mental illness receive treatment there, normally for
milder conditions, although some of these are later referred for
Van Hoof et al, Outpatient care; time series of beds from Eurostat Health
Database.
4
Fred Zijlstra, “Netherlands”, in Chiara Samele et al, eds., Mental health
Systems in the European Union Member States, 2013; Alessia Forti et al,
“Mental Health Analysis Profiles: Netherlands”, OECD Health Working Papers,
No. 73, 2014. This latter report contains the best, detailed description of the
Dutch mental health system in English.
5
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
other care.6 Primary care usually comes directly from a GP, but
primary-care psychologists are also available. A large number
of GP surgeries also have a specialist mental health nurse and
some have primary-care mental health social workers.7
Further promoting the integration of primary care, as
well as other non-psychiatric medical personnel, into the
mental health provision has also been a programme—
originally government funded, but since taken on by the
Dutch Psychiatric Association—of creating detailed, multidisciplinary treatment guidelines for a range of mental
illnesses. Drawing on input from ten patient and carer bodies,
as well as 30 professional organisations, it has since 1999
produced 18 sets of guidelines on conditions ranging from
anxiety disorders, depression, and schizophrenia through
mental health considerations in the event of a major shock.
Although well-known within Dutch medicine, the integration
of the guidelines into practice has been slow—so far, 28%
of relevant professionals use them consciously in daily
practice—but this is expected to grow.8 This effort is also
part of a broader tendency to create effective care paths for
individual conditions. Dr Keet explains that most mental
healthcare is organised in this way. This has the strength of
providing evidence-based treatment, but can lead to overly
close attention on a specific condition, rather than on the
needs of the person as a whole, in the majority of cases where
co-morbidities exist.
A well-staffed system but one that raises cost
concerns
As the Index shows, the mental healthcare provision that
has resulted from this evolution offers high levels of access.
The Netherlands’ seventh-place ranking in The Economist
Christina van der Feltz-Cornelis et al, “Treatment of mental disorder in the
primary care setting in the Netherlands in the light of the new reimbursement
system: a challenge?”, International Journal of Integrated Care, 2008.
6
Intelligence Unit’s Index is helped by the country’s firstplace finish in the category for the number of mental health
personnel. With the sixth-highest figure for the number of
psychiatrists per head, as well as the second-highest for both
specialist social workers and psychiatric nurses, the Dutch
have a range of expertise in the system. Dr Keet believes that
“we have a sufficient number of professionals and facilities, as
well as funds, to provide care”. He adds, however, that the high
number of beds using up resources impedes their more efficient
use.
Perhaps ironically, one of the most controversial issues
surrounding mental healthcare in the Netherlands arises from
people actually seeking treatment. The proportion of health
spending dedicated to mental health rose from around 3% in
the year 2000 to 11% by the end of the decade.9 The problem
has not been an increase in the levels of mental illness in the
country, nor even a relative rise in the costs of mental health
treatments, which have gone up at about the same rate as other
medical care. Instead, notes Mr van Hoof, the “numbers are
about growth of use”. Throughout the last decade the number
of individuals seeking treatment for mental health has risen;
currently, about 6% of the entire population do so, and 5% have
some type of secondary care.10
On the one hand, this is positive. The treatment gap, although
still substantial, has declined and spending in the area of
mental health overall tends to be cost-effective in the long
run. On the other, the trend has created a need for immediate
outlays in a time of austerity. Accordingly, Mr van Hoof notes
that “cost has been an issue and led to major reforms of mental
healthcare in the Netherlands”. In some cases, this has led
to knee-jerk responses, such as a co-payment introduced in
2012 on secondary mental health services in order to reduce
Figures from World Health Organisation (WHO), Atlas Mental Health
Resources in the World, 2001; WHO, Mental Health Atlas, 2011.
9
10
8
Derived from GGZ Nederland, “Key Figures 2012”, and population data.
Forti et al, “Netherlands”.
7
Forti et al, “Netherlands”.
4
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
their use, a measure repealed a year later. Nevertheless, in
2013, Philippe Delespaul, the new chair for innovation in Dutch
mental healthcare at the University of Maastricht warned that,
given ongoing funding restraints, the current system would
not be able to expand to meet the needs of the three-quarters
of the population who are likely to need some mental health
treatment at some point in their life. Instead, he pointed to
greater use of multi-disciplinary, community-based care and a
reduction in bed numbers as the route to lower cost, but more
effective, provision.11
Thus, cost consciousness pervades much thinking around
mental healthcare and service provision in the Netherlands.
It even explains the Netherlands’ most striking weaknesses
revealed in the Index data: the country usually has a strong
human-rights record, but is ranked last for its adherence to
treaties that are relevant to the rights of those living with
mental illness. Although the Dutch government has signed
the Convention on the Rights of Persons with Disabilities
(CRPD) in 2007, it has yet to ratify it. It has also not signed
the optional protocol to that treaty allowing individuals and
groups to take relevant complaints to the UN Committee on the
Right of Persons with Disabilities. Yet, this is inconsistent with
other Index indicators: the Netherlands has introduced—in
accordance with the CRPD—supported decision making and
has moved away from guardianship; it does not take custody
of children away from parents living with a mental illness
solely because of their condition; and it has extensive review
bodies to protect the rights of service users. Instead, the
delay in ratification (the government expects to do so in 2015)
has arisen from the need to determine the extent and cost of
changes to the law that will be required under the Convention.
Adjusting to a new funding system
Mental healthcare provision in the Netherlands has also been
affected by a major reform of the Dutch healthcare system
in 2006, which the government enacted to address rapidly
increasing healthcare spending overall. These put in place an
insurance-based funding system. Residents must purchase
health insurance from one of a range of competing providers.
The government sets minimum requirements for these policies,
and prices, so insurers differentiate themselves on quality of
care. They in turn commission care from providers—almost
entirely private—who need to compete based on price and
quality. The government plays a regulatory, oversight role, but
is not directly involved.
Accompanying this general reform, mental health saw
important specific changes. As a result, mental health services
are now covered under the basic insurance system, which
pays for all outpatient and community care and inpatient care
lasting less than one year. This provides the large majority of
funding, in 2012 making up 72% of non-forensic mental health
spending. The only remaining AWBZ-related involvement
is funding of longer-term inpatient care, which comprises
26% of the total. The very small remainder is paid out of the
statutory social services budget, which is funded nationally but
controlled by local authorities.12 Meanwhile, as before, nonmedical services, such as employment and housing, are the
responsibility of other government departments.
(I) Negative implications
The new arrangement has pros and cons. One of the downsides,
says Mr van Hoof, is that the increased fragmentation of
Philippe Delespaul, “Inaugurale rede ‘Innovatie in de Geestelijke
Gezondheidszorg’”, 2013.
11
12
5
Derived from GGZ Nederland, “Key Figures 2012”.
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
budgetary responsibility, especially in the absence of a strong
national policy, is likely to slow integration. “It is easy to shift
responsibilities, for community authorities [administering
social support funding] to say ‘this is healthcare,’ or insurers
to say, ‘this is social care’, when the needs of those with
mental illness always straddle different areas. You need
clear reimbursement systems that reward co-operation.” In
particular, he notes that the current funding arrangements
are unlikely to promote co operation or the development of
comprehensive and coherent community support services and
systems.
Another important issue arises from a weakness in the marketbased nature of the new system: those with serious mental
illness lack extensive market power. The reforms, notes Dr
Keet, “stimulated many organisations, but they competed on
services for those with moderate disorders”. This, in itself is
not bad: these conditions need treatment and treating early
can help prevent them worsening. On the other hand, it is
not sufficient to address all the needs of the population. Dr
Keet adds that “There has not been much gain for those with
severe mental illnesses. Competition will not be for provision
of care for those who need it most.” Mr van Hoof agrees: “A lot
of capacity is directed at people with mild problems. People
with severe problems get good care, but little psychological or
psychotherapeutic treatment, so there is a gap.” Both say that
a lack of national policy and active government involvement in
mental health contributes to this ongoing deficiency.
(II) Positive innovations and co-operation
The absence of a strong national policy, dating back to before
the health reforms, also has positive aspects. Dr Keet explains
that “there is space for local initiatives”. A number of these
13
For a detailed discussion of FACT, see the main Economist Intelligence Unit
white paper arising from this project, Mental Health and Integration.
14
Christina van der Feltz-Cornelis et al, “The Depression Initiative. Description
of a collaborative care model for depression in the primary care setting in the
Netherlands”, Clinical Neuropsychiatry, 2011; KM Huijbregts et al, “A targetdriven collaborative care model for Major Depressive Disorder is effective
6
initiatives show substantial promise to reshape mental health
and social care even beyond the Netherlands.
Probably the best known is Flexible Assertive Community
Treatment (FACT). Traditional ACT care provides a range of teamprovided, intensive, home- and community-based care and
services to those most at risk. FACT retains this element of care,
but adds less intensive provision for those whose condition is
more stable and a flexible way to switch users between the two
groups should their individual situation change. The system is
effective: one study in the southern Netherlands saw remission
rates go from 19% to 31% after its introduction. FACT began
with experimentation in a single regional health unit in 2003
and then spread. Dr Keet notes that its rapid development—150
certified FACT teams now serve around 15% of those with
severe or long-term conditions—has resulted from “a very
strong bottom-up movement of integrated care. It was not a
part of government health policy, but was typically Dutch in
that something bottom-up has become well organised with
extensive certification.”13
FACT provides secondary care, but other stakeholders have
been innovating in primary care. The Trimbos Instituut, funded
by various health insurers, has led efforts to adapt to mental
healthcare the principles of collaborative care used successfully
in somatic chronic conditions. The Depression Initiative began
in 2006. It is centred around a care co ordinator—typically
a specialist psychiatric nurse—who monitors the patient’s
condition according to multi-provider guidelines with the help
of specialist software. Working with the patient and taking
into account his or her preferences, the co-ordinator interacts
with other healthcare professionals—usually a GP, but also
occupational therapists and hospital outpatient doctors—to
adjust the treatment plan where necessary. In small evaluation
in primary care in the Netherlands. A randomized clinical trial from the
depression initiative”, Journal of Affective Disorders, 2013; M Goorden et al,
“Cost-utility analysis of a collaborative care intervention for major depressive
disorder in an occupational healthcare setting”, Journal of Occupational
Rehabilitation, 2014; Forti, “Netherlands”.
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
trials the approach resulted in better outcomes than those
seen in usual treatment in primary care, but seemed to have
little effect on occupational therapy. Results were sufficiently
positive, however, that plans exist to create a similar scheme
for anxiety disorders.14
Finally, the Dutch have been active in experimenting with
e-mental health—the provision of care over the Internet or
phone. In 2010 some 181,000 people, or more than 1% of the
entire population, received online help for depression or eating
disorders. So far, little evidence on cost-effectiveness exists,
but the field is expected to grow either on its own or as an
adjunct to more traditional care.
Besides allowing innovation, another positive aspect of Dutch
mental healthcare is that, diverse stakeholders have become
used to working together to address problems. In 2011 the
industry group for Dutch mental healthcare providers, the GGZ,
renewed its successful 2003 agreement with police authorities
that covers areas such as information exchange and joint
protocols outlining how to help those with a mental illness
who come into contact with the police. An important result has
been the participation of mental health providers in the Dutch
Safe House programme. There are currently 41 of these offices,
where networks of local police, justice, social care, health, and
mental health professionals meet to discuss the most effective
joint, integrated interventions for individuals in the community
with complex needs who represent a severe public nuisance or
are repeat offenders.
Similarly, in 2012 the GGZ signed a co-operation agreement
with the Employee Insurance Agency, the national social
benefits office, to help joint clients either to retain or find
new employment as easily as possible. In doing so, the Index
7
shows that the Dutch can build on an already strong record:
the country places fifth in the “Opportunities” category and
is one of the leaders in putting in place Individual Placement
Services (IPS), a type of scheme for finding and keeping work
that involves training after placement and that has been shown
to be more effective than traditional “train and place” schemes.
That said, as Dr Keet points out, there is a need for more
professionals to provide IPS services.
The most extensive example of co-operation, though, has
been the Administrative Agreement on the Future of Mental
Healthcare. Negotiated and signed in 2012 by the Ministry
of Health, the GGZ, patient and carer groups, the insurers’
trade body, and several societies representing mental health
professionals, the document contained an extensive set of
goals for the sector for 2013 and 2014. Part of the effort
invariably revolved around cost containment, keeping overall
price increases below 2.5% in 2013 and 1.5% in 2014, but it
also involved a number of important reforms. These include
new funding measures and care pathways to increase further
the role of GPs and primary-care psychologists in patient care,
and to reduce that of specialists by 20%; a greater emphasis on
data gathering and its use in shaping evidence-based care; and
the creation of an anti-stigma campaign, which has come into
being as Samen Sterk Zonder Stigma (Together Strong Against
Stigma).
The agreement shows that market forces can also have positive
effects on mental health provision. In addition to the greater
push towards primary care and better data use—both of which
promote better care at lower cost—one of its most important
goals is a 30% reduction in psychiatric hospital beds. Despite
their relatively small role in the overall offerings of the sector,
hospitals take up nearly 60% of all mental health funding.
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
Reducing their role and number would therefore decrease costsubsidisation, enabling lower-priced provision overall. Mr van
Hoof notes that “commercial insurers have taken the lead in
[pressing for] psychiatric bed reduction and are forcing mental
health providers to cut them. This is not bad, we have a lot of
beds.” He worries, however, that these savings may not end
up being put towards better community care, but rather would
result in a net cut in spending. “The figures are not available
yet,” he adds.
The same system that promotes this laudable record of
innovation, however, makes their universal roll out more
difficult. Dr Keet believes that “We have pockets of excellence,
but the lack of a national policy means that this is not true all
8
over the country.” Mr van Hoof adds, “There are some good
developments in the field of mental healthcare—especially
FACT, which is spreading quite rapidly. They are difficult to
implement, but we are making progress. We have money and
we think we have know-how, but we are lacking the proper
incentives and conditions on a national policy and system
level.”
Overall, then, the evolution and funding of Dutch mental
healthcare has led to a relatively effective system, but one so
distinct from those of its neighbours as to provide few systemwide lessons for other European countries. Nevertheless, it has
become a source of numerous interesting innovations worth
watching.
© The Economist Intelligence Unit Limited 2014
Mental health and integration
Provision for supporting people with mental illness: A comparison of 30 European countries
About the research
This study, one of a dozen country-specific articles on the
degree of integration of people with mental illness into
society and mainstream medical care, draws on The Economist
Intelligence Unit’s Mental Health Integration Index, which
compares policies and conditions in 30 European states.
Further insights are provided by two interviews—with Frank
9
van Hoof, senior scientist at the Trimbos Instituut, and Rene
Keet, a psychiatrist and director of the Mental Health Centre,
GGZ North Holland—along with extensive desk research. The
work was sponsored by Janssen. The research and conclusions
are entirely the responsibility of The Economist Intelligence
Unit.
© The Economist Intelligence Unit Limited 2014