Chapter 088. Hepatocellular Carcinoma (Part 6) pptx
Bạn đang xem bản rút gọn của tài liệu. Xem và tải ngay bản đầy đủ của tài liệu tại đây (31.32 KB, 5 trang )
Chapter 088. Hepatocellular
Carcinoma
(Part 6)
Hepatocellular Carcinoma: Treatment
Most HCC patients have two liver diseases, cirrhosis and HCC, each of
which is an independent cause of death. The presence of cirrhosis usually places
constraints on resection surgery, ablative therapies, and chemotherapy. Thus
patient assessment and treatment planning have to take the severity of the
nonmalignant liver disease into account. The clinical management choices for
HCC can be complex (Fig. 88-1). The natural history of HCC is highly variable.
Patients presenting with advanced tumors (vascular invasion, symptoms,
extrahepatic spread) have a median survival of ~4 months, with or without
treatment. Treatment results from the literature are difficult to interpret. Survival is
not always a measure of the efficacy of therapy because of the adverse effects on
survival of the underlying liver disease. A multidisciplinary team, including a
hepatologist, interventional radiologist, surgical oncologist, transplant surgeon,
and medical oncologist, is important for the comprehensive management of HCC
patients.
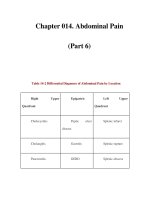
Figure 88-1
Treatment approach to patients with hepatocellular carcinoma.
The
initial clinical evaluation is aimed at assessing the extent of the tumor and the
underlying functional compromise of the liver by cirrhosis. Patients are classified
as having resectable disease, unresectable disease, or as transplantation
candidate
s. Abbreviations: OLTX, orthotopic liver transplantation; TACE,
transarterial chemoembolization; PEI, percutaneous ethanol injection; RFA,
radiofrequency ablation; LN, lymph node. Child's A/B/C refers to the Child-
Pugh
classification of liver failure.
Stages I and II HCC
Early-stage tumors are successfully treated using various techniques,
including surgical resection, local ablation (thermal or radiofrequency), and local
injection therapies (ethanol or acetic acid). Because the majority of patients with
HCC suffer from a field defect in the cirrhotic liver, they are at risk for subsequent
multiple primary liver tumors. Many will also have significant underlying liver
disease and may not tolerate major surgical loss of hepatic parenchyma; they may
be eligible for orthotopic liver transplant (OLTX) in the future. An important
principle in treating early-stage HCC is to use liver-sparing treatments and to
focus on treatment of both the tumor and the cirrhosis.
Surgical Excision
The risk of major hepatectomy is high (5–10% mortality) due to the
underlying liver disease and the potential for liver failure. Preoperative portal vein
occlusion can sometimes be performed to cause atrophy of the HCC-involved lobe
and compensatory hypertrophy of the noninvolved liver, permitting safer
resection. Intraoperative ultrasound is useful for planning the surgical approach. In
cirrhotic patients, any major liver surgery can result in liver failure. The Child-
Pugh classification of liver failure (Chap. 295) is a reliable prognosticator for
tolerance of hepatic surgery, and only Child A patients should be considered for
surgical resection. Child B and C patients with stages I and II HCC should be
referred for OLTX if appropriate, as should patients with ascites or a recent history
of variceal bleeding. Although open surgical excision is the most reliable, the
patient may be better served with a laparoscopic approach to resection, using RFA
or percutaneous ethanol injection (PEI). No adequate comparisons of these
different techniques have been undertaken, and the choice of treatment is usually
based on physician skill.
Local Ablation Strategies
Radiofrequency ablation (RFA) uses heat to ablate tumors. The maximum
size of the probe arrays allows for a 7-cm zone of necrosis, which would be
adequate for a 3- to 4-cm tumor. The heat reliably kills cells within the zone of
necrosis. Treatment of tumors close to the main portal pedicles can lead to bile
duct injury and obstruction. This limits the tumors that are anatomically suited for
this technique. RFA can be performed percutaneously with CT or ultrasound
guidance, or by laparoscopy with ultrasound guidance.